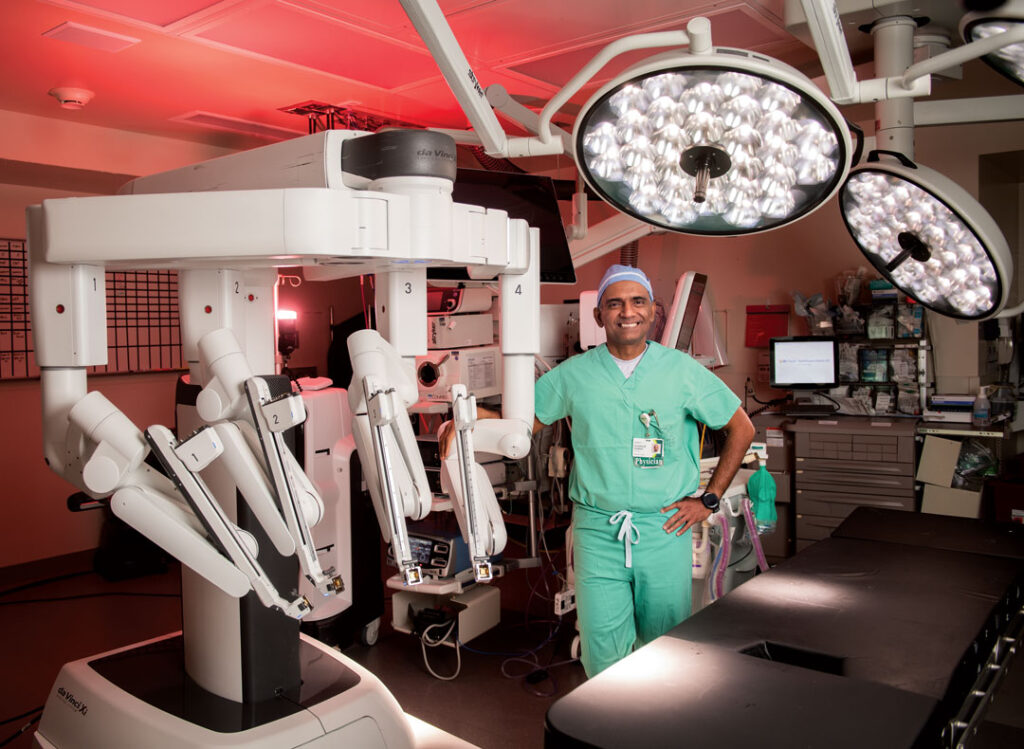
A Closer Look: Karl Keeler
President, Mercy Medical Center-Des Moines

JOE GARDYASZ May 15, 2018 | 8:25 pm
8 min read time
1,816 wordsBanking and Finance, Business Record Insider, Health and WellnessKarl Keeler has held executive leadership positions at hospitals across the United States, but his new role at Mercy Medical Center-Des Moines enabled him to return to both Mercy and to Iowa. Keeler began as Mercy-Des Moines’ new president on Jan. 15, filling the role vacated by Bob Ritz, who was promoted to president and CEO of Mercy Health Network. Early in his 24-year career, the Utah native worked for hospital systems in St. Louis and Denver. While he was chief operating officer of Mercy-Cedar Rapids, Keeler helped keep the hospital system functioning and responsive through the historic 2008 flood and the subsequent cleanup and recovery efforts. For the past seven years, Keeler was president of Saint Alphonsus Medical Center in Nampa, Idaho, where among his accomplishments he led a $180 million replacement facility project. He acknowledges having a fiercely competitive streak and enjoys flying down snowy hills on skis, roaring along twisty mountain roads on his motorcycle, or taking on any activity that involves going fast. He and his wife, who is a nurse, recently moved to Waukee with their three boys and two girls.
How did you get interested in health care?
I was in the backyard with my brother and a bunch of the neighborhood kids and we were playing football. I was 12 or 13, and he was a couple of years younger than me. I was playing quarterback and I went back for a pass, and threw a beautiful spiral. He dove to get it, landed on a metal sprinkler and just sliced his knee open from side to side. You could see everything, from the muscle to the fat. I was hooked; I said, “This is what I want to do with my life.”
What made Mercy-Des Moines an attractive career move?
One, it’s an excellent organization. When you move from [another Mercy organization] you know you’re going to a great organization that has a long history of excellent quality. The state of Iowa overall has excellent health care quality; it’s always been ranked in the top few for outcomes. … It’s kind of like coming home — I was at Cedar Rapids for six years, so I know that area well. I had been to Des Moines a number of times. It was just the right fit.
What was it like going through the flood in Cedar Rapids?
The people just came together, and it’s really a community. We knew that we were going to have flooding, and we had our emergency plan together on how we were going to help others in the community, but we didn’t know that [the hospital would be directly affected]. We sent, I think, 186 patients to 30-plus hospitals across the state, so just the coordination of care was phenomenal. The staff were just amazing in the face of disaster. The community came out and helped us to sandbag. … It’s a perfect definition of why we wanted to come back here. … And I’m so happy that Mercy-Des Moines is high up on a hill.
What priorities do you have for your first year?
Only being here a couple of months, with about 7,000 employees and 70 locations, first off I’m just trying to learn and listen. We’ve provided great care here for over 100 years, and we want to figure out how we maintain that. For instance, we just launched a digital app that you can use to connect with a provider through your phone. So we’re looking at all the ways we can connect. We have over 20 health coaches that are part of our clinically integrated network that actually work to keep you out of the hospital. So we’re not just looking at being a hospital organization anymore, we’re looking at how do we actually serve the population — how do we keep you well and out of the hospital. When people do need our services in the hospital, we are actually seeing higher-acuity patients. Our ICUs are actually full all the time now, so we are caring for that higher-need patient as well.
We have three priorities we’re really focused on. One, we’re focused on our employee engagement. How do we really help each other to be successful? The second is on our patient experience. It’s really about how we’re providing a world-class patient experience, and that includes all the quality [measures] — the things that you expect when you come to us. The third is our stewardship. If you look at our cost per capita for health care, we’re actually one of the lowest states in the country. But health care is expensive, so how do we manage those resources, and how do we individualize care to help meet your needs and achieve your goals?
Are the affordable care organizations proving to be the right model going forward?
There are many ACOs that are not successful. I think ours are, because we had a great base already with our Mercy Care Clinics and had been working on our patient-centered medical home and population health in this state since the mid- to late-2000s. Even in Boise, we weren’t looking at that until 2013 or 2014. Iowa has definitely been a leader. And Dr. [David] Swieskowski, who was over our Mercy Clinics and now leads our ACO, has been a leader and [Mercy ACO has] been recognized for the ACO work they’ve done. That’s important, because it’s about coordinating your care, and not just when you’re sick but more importantly when you’re well. We have about 350,000 patients that are part of our ACO that we care for from a contracting perspective.
If there was just one key thing you could change about how health care is delivered, what would it be?
If I had my magic wand … having the electronic health record is sometimes a barrier. If I could just change that so it’s 100 percent intuitive and you could see all the key pieces so you could have the exact insight into your own body and how it’s performing. … Most of health care is personal choice — there are lots of things we can do to get you back to health, but the reality is, it’s what you eat, it’s what you drink, it’s your genetics. Those kinds of things have more effect than anything health care can actually do. So if I had a magic wand, it would be to try to have a better tool to help not only us work with you on your health, but also to help you personally to make sure you are as well as you want to be.
There has been a lot of discussion and awareness in Iowa about mental health care access. Your thoughts on Mercy’s role in mental health care?
That is a difficult issue, and every community I’ve been at has the same problem. … We have a team that’s actually working on what we’re looking at in the future, so hopefully in the next couple of months we’ll have something out about what our ultimate plan is. … We have been working collectively with UnityPoint Health to see what we can do together. … Unfortunately because there aren’t enough [psychiatric] beds we have people waiting for hours and hours. We are starting a behavioral health residency program [to train new psychiatrists] beginning July 1, because that’s another problem — we just don’t have enough care providers. [After this interview was conducted, Mercy filed a letter of intent on May 4 saying it plans to seek state approval to build a 100-bed psychiatric hospital in Polk County.]
Any civic organizations that you plan to connect with?
We’re a community and service organization, so I expect all my leaders to do that as well to give back to the community. I’ve been on many, many boards. In Cedar Rapids I was on the United Way board; I’ve been on the American Cancer Society board and other boards. Every place I go I try to serve on the community boards. In Idaho, I was on the foundation board for the College of Western Idaho, the chamber of commerce board and the American Cancer Society Board. My wife had breast cancer when she was 30, so we’re big fans of the Cancer Society.
What else is on your mind?
Health care is a lot harder now than it was 15 years ago — think just from the pressure of cost: How do we make sure we make it affordable, but have all the services that people want right now? The reality is that managed Medicaid has been a decrease in funding for us. Medicare [payment rates] go up by 1 percent, but our cost of living goes up a lot more than that. People want raises, and we are looking at new technology, we have [aging facilities] and even just the [cost of] regulation is a factor. Fifteen years ago, our quality department was really focused on quality; now it’s focused on making sure we collect the data needed for all the regulations — the administrative burden is just so much greater. … And we’re one of the lowest [Medicare] reimbursed states, which makes it even more difficult. The weird thing is, the better quality that you have, you get paid less from a Medicare perspective.
Yet you still get up and go to work every day?
I love it, and I love it because what I do can really actually help people. … If we can do it right, it actually helps people improve their lives. So it fits my own personal mission around helping people and service, and I get to do that every day.
Tell me about your family.
My wife is a nurse, so being in health care and an administrator, she’s actually a great sounding board to say, “Hey, that’s not going work,” or “That’s a great idea.” We have five kids. The oldest is 17, then 15, 13, 9 and 5. Three boys, two girls. We have a busy household. All the boys are into soccer and the girls like soccer and dance.
Since you mentioned you were once a Forty Under 40 in Cedar Rapids, what’s an interesting fact that not many people know about you?
We like the outdoors — all of our family rides dirt bikes. So we have a stable of motorcycles that we ride. And there’s a guys’ trip that I go on — there’s about 12 to 18 of us from all over the country that get together once a year in the fall and ride a different place in the country. Last year it was Moab. I’m kind of an extreme sports guy — I grew up skiing. I’m kind of a thrill-seeker, and my kids are that way, too. They love anything that’s fast, from roller coasters to skiing to whatever.