Workforce a top priority as Iowa aims to improve mental health services

Kyle Heim May 31, 2024 | 6:00 am
7 min read time
1,769 wordsBusiness Record Insider, Health and WellnessWhile COVID-19 accelerated the push into more virtual mental health care service opportunities, a significant challenge began surfacing: hiring.
In 2012, 236 licensed psychiatrists were practicing in Iowa, according to the Iowa Health Professions Tracking Center at the University of Iowa Carver College of Medicine.
By 2021, that number dipped 10.17% to 212, despite 1 in 5 adults in Iowa, or about 600,000, living with some form of mental illness, according to the National Alliance on Mental Illness (NAMI) North Iowa.
Meanwhile, 66% of the state’s professional psychiatrists work in Johnson, Linn and Polk counties, while 73 of Iowa’s 99 counties do not have a psychiatrist.
A report released earlier this year by the Treatment Advocacy Center showed that Iowa ranks last in the United States for the number of state psychiatric beds per 100,000 residents. It had 64 state-managed in-patient beds to treat adults in 2023, equating to two beds per 100,000 residents.
The report states that 50 beds per 100,000 people are required to provide “minimally adequate treatment” for people with severe mental illness.

“That report recognizes the number of state-operated mental health beds,” said Kelly Garcia, director of the Iowa Department of Health and Human Services. “It’s not overall bed capacity; it’s state-operated bed capacity. And yes, we do have the lowest number per capita. That’s not a bad thing. … What [the report] articulates is that there is no one answer to solving our national mental health crisis, or in this case, behavioral health, in some aspects, crisis. So state-funded beds are not the only answer.
“And what we would look at as a system is more specialized capacity, but it’s a full array of services across the board at every level of that continuum of care. So our state-run facilities, which we call specialty care, would be at the highest end. We’re a safety net provider; we take the most complex patients in the state.”
Iowa has two state-operated health institutes – Cherokee Mental Health Institute, which primarily serves adult patients and forensically involved patients, and Independence Mental Health Institute, which serves youths.
The Cherokee location focuses on providing competency restoration work to patients, which Garcia said had previously been a gap in Iowa.
“We identified that gap, and we recommended specializing our care so we really had focus,” she said. “We have seen tremendous success in that movement. We went from having a backlog of those patients who are in jail and need a competency restoration to stand trial to no longer having a backlog and instead having a manageable list of individuals come into our care and come back out.”
In an effort to improve care at the Independence Institute, separate wards were designed for children and adolescents.
“We now have a child and an adolescent ward separated out because 5- and 6-year-olds have different needs than 15-year-olds, and that has proven to be an incredible success,” Garcia said. “… Across child welfare programs in the nation, there is what I would call an epidemic in terms of children not having placement, meaning that they are sleeping in child welfare offices every night because there is no place to put them.
“We recently have been invited to be part of a national network in terms of dialoguing on how to solve this work. And the reason why is because we don’t have kids living in offices in the state; we are rare in that.”

Ryan Crane, executive director of the National Alliance on Mental Illness (NAMI) Iowa, said that even though Iowa has the fewest number of state-operated psychiatric beds per 100,000 residents, there often isn’t enough staff available to cover the number of beds in the state.
“There’s been a lot of ink spilled that we have a shortage of beds in this state, and that is objectively true,” Crane said. “A kind of interesting nuance on that, and Kevin Pettit at Clive Behavioral Health had some interesting things to say about this, too, just as an employer, that sometimes we actually have empty beds on a given day because we can’t find the right staffing ratios. Per capita, we don’t have as many beds as most other states, but even within that statistic is this tough nugget that we don’t have enough workers even for those that we do. Workforce is a significant challenge in that regard.”
Coinciding with a sudden drop in the health care workforce in the last decade was a rapid expansion of telehealth services. The use of tele-visits, including video and phone visits, increased from 14% in 2016 to 28% in 2019 to 80% in 2022, according to the National Institutes of Health, creating more remote positions and expanding the locations where workers could live.
“While our world was really opened up through the virtual spaces that we now are able to occupy, and that has been a really remarkable change, it’s also made hiring more challenging because your opportunities can be pretty endless,” Garcia said. “You can live in a lot of different spaces and work remotely. That’s been a really interesting shift, but it’s been one where I think a number of sectors were caught a little bit flat-footed.”
No ‘silver-bullet’ solution
Garcia added that there isn’t a “silver-bullet” solution to solving the health care workforce shortage in Iowa and that leaders need to think in a multifaceted way to ensure Iowa remains nimble, flexible and future-focused around how to manage in the post-COVID era.
One of the focuses for the Iowa Department of Health and Human Services has been working with partners on intentional recruitment strategies.
“We work really closely with the University of Iowa, and we work with Des Moines University here in clinical programs,” Garcia said. “One of the ways that we can help is to think about clinical rotations in our workforce and the spaces that we occupy. We are currently participating with the University of Iowa to have a psychiatric residency rotation at our facilities. We are a specialty care provider in the state, so we have some incredibly complex individuals that make for a great training ground in the facilities that we occupy and operate.
“As those residency rotations come through, not only do we gain the benefit of having a steady workforce, but then oftentimes what we see is that those clinicians, in this case doctors, fall in love with the work, they love the complexity of the work, they love rural Iowa, so they stay. And that is a pipeline-building capacity. We’re doing that in a number of spaces, and we’re thinking about it not just at the top end of that clinical spectrum, but we’re thinking about it in terms of direct care workforce as well.”
Another area of focus and possible incentive to recruit health care providers has been loan repayment.
“That is one strategy that tends to work, and we have active conversations with [Executive Director Beth Townsend] over at Iowa Workforce Development and our partners in the Legislature as well,” Garcia said. “This is an area that [Gov. Kim Reynolds] is really keenly interested in, thinking about how we take individuals who are interested in a subject matter really early on in their education and how we get them in direct pipelines, thinking all the way in high school. And we have seen some great successes there across health care – they’re very obvious – but also on the human services side as well. We’re working on some child care spaces there, and that continues to be a national issue.”
In an effort to improve access to mental and behavioral health services, Reynolds recently signed into law House File 2673, which combines Iowa’s mental health and substance use regions into seven unified behavioral health districts. It also places disability services under the jurisdiction of the Iowa Department of Health and Human Services.
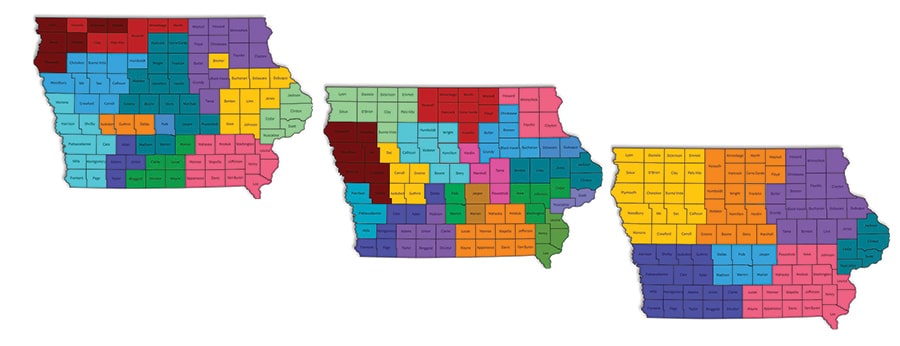
The map on the left shows where Iowa’s 13 current mental health and disability service regions are concentrated. The map in the middle shows where Iowa’s 19 Integrated Provider Networks that manage substance use disorder and problem gambling services are located. The map on the right shows the seven proposed behavioral health districts in House File 2673, which was signed into law by Gov. Kim Reynolds on May 15. Source: Iowa Department of Health and Human Services.
Each district will be required to provide a standard set of core services, ensuring consistent care systemwide, Reynolds said during a bill signing on May 15. The districts are expected to provide education, prevention, early intervention, treatment, recovery and crisis services related to mental health and substance use disorders.
“I think that both as a spokesman of NAMI and as somebody who’s been doing advocacy work of different kinds for 15, 16 years in the state of Iowa, I just think that combining those two things is really savvy,” Crane said. “And I am excited about what can happen when substance use and mental health start talking more closely and stop kind of arbitrarily defining themselves to each other. … This streamlining and this realignment is just the next iteration in trying to do better.”
While the bill had clear bipartisan support in the state Legislature and received support from the Iowa Hospital Association, Iowa Mental Health Advocacy, NAMI Iowa, the Coalition for Family and Children’s Services in Iowa and others, according to the Cedar Rapids Gazette, there are still some concerns.

“Anytime a system changes, we worry most about the people we are serving, our employees and the need to maintain the continuity of care to our clients,” Flora Schmidt, executive director of the Iowa Behavioral Health Association, wrote in a statement to the Business Record. “At this time, we continue to have more questions than answers as we await the enactment of the legislation, the release of the Iowa Dept. of Health and Human Services transition plan, as well as the forthcoming stakeholder engagement opportunities and the development of the Behavioral Health Service System State Plan.
“IBHA is cautiously optimistic about the overall alignment, transition and continuity of services, and changes within this new Behavioral Health Service System. Our primary concern at this point is the proposed timeline moves too fast to seamlessly create, design and integrate legacy programs/services within the new structure. We also want to make sure this is truly an integrated behavioral health system for not only mental health, but that also meets the unique needs of those with substance use disorders, including assurances there is adequate funding for specialized programs for women, children and adolescents, as well as residential treatment and prevention services.”

Kyle Heim
Kyle Heim is a staff writer and copy editor at Business Record. He covers health and wellness, ag and environment and Iowa Stops Hunger.